Mindfulness Meditation: Healing Kids with Dissociative Disorder
Dissociative disorder in young children, often stemming from trauma, causes them to detach from real…….
In the intricate landscape of child mental health, Therapies aimed at addressing Dissociative Disorder in young children stand as a beacon of hope for countless families worldwide. This comprehensive article delves into the intricacies of this specialized therapeutic approach, exploring its mechanisms, global reach, economic implications, technological integrations, and the challenges it faces. By examining these facets, we aim to provide a holistic understanding of Therapy for Young Children Dissociative Disorder (TYCDD) and its profound impact on fostering resilience and restoration in affected individuals. Through this journey, readers will gain insights into the intricate world of child psychology, therapeutic interventions, and the collaborative efforts required to nurture vulnerable young minds.
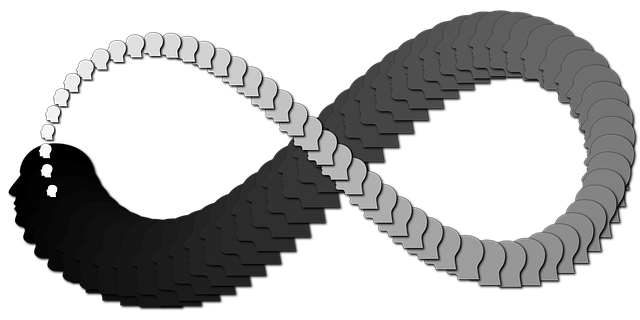
Therapy for Young Children Dissociative Disorder is a specialized form of psychotherapy designed to assist children aged 5-12 years old who suffer from dissociative symptoms, often stemming from trauma. Dissociation refers to a complex psychological mechanism where an individual disconnects from their thoughts, memories, feelings, or sense of identity as a coping response to overwhelming stress or trauma. This disorder manifests in various ways, including detached behavior, amnesia, and altered states of consciousness.
The core components of TYCDD encompass:
Psychoeducation: Educating both the child and their family about dissociation, its causes, and its impact, fostering understanding and encouraging active participation in therapy.
Trauma-Focused Therapy: Utilizing evidence-based approaches like Eye Movement Desensitization and Reprocessing (EMDR) or Cognitive Behavioral Therapy (CBT) to help children process traumatic memories and develop healthy coping strategies.
Play Therapy: Leveraging play, art, and other creative mediums to enable children express themselves, explore emotions, and internalize therapeutic concepts in a safe, non-threatening manner.
Family Involvement: Engaging parents and caregivers in therapy sessions to enhance their understanding of dissociation, improve family dynamics, and provide support strategies for managing the child’s condition at home.
The field of child psychology has witnessed a growing recognition of dissociative disorders since the late 20th century. Early approaches focused primarily on adult populations, but with increasing research and awareness, therapists began to adapt existing therapeutic modalities to cater to younger patients. The development of TYCDD can be traced back to pioneering work by psychologists like Bessel van der Kolk, who emphasized the impact of trauma on children and advocated for specialized interventions.
TYCDD holds significant importance in several ways:
Therapy for Young Children Dissociative Disorder has gained global recognition, with professionals across diverse cultural settings adopting and adapting this therapeutic approach. The Universal Nature of trauma and dissociation as psychological responses to stressful events ensures a broad applicability for TYCDD. However, cultural nuances and varying healthcare systems present both challenges and opportunities in its implementation.
Growing Awareness: Increasing awareness about childhood trauma and mental health issues has led to greater demand for specialized therapies like TYCDD.
Cultural Adaptation: Therapists worldwide are tailoring TYCDD to suit local cultural contexts, ensuring sensitivity to traditional beliefs and practices while delivering evidence-based care.
Integration with Technology: The digital age has seen the integration of technology in TYCDD, including online therapy platforms, virtual reality (VR) for exposure therapy, and mobile apps for psychoeducation and monitoring progress.
Collaborative Care Models: There is a growing trend towards collaborative, multidisciplinary care models involving psychiatrists, psychologists, social workers, and primary care providers to optimize treatment outcomes.
The impact of TYCDD varies across regions due to differences in healthcare infrastructure, cultural attitudes, and socioeconomic factors:
| Region | Impact Factors | Examples |
|---|---|---|
| North America | Advanced healthcare infrastructure, high awareness | USA: The Child Mind Institute offers specialized programs for dissociation. |
| Europe | Diverse healthcare systems, strong mental health advocacy | UK: The National Health Service (NHS) provides access to TYCDD through specialized clinics. |
| Asia | Cultural sensitivity, growing mental health initiatives | Japan: Traditional therapeutic approaches blend with modern techniques for treating dissociation in children. |
| Africa | Limited resources, cultural barriers | South Africa: Non-profit organizations offer community-based TYCDD programs despite resource constraints. |
The global mental health market, including therapies for dissociative disorders, is experiencing significant growth. This expansion is driven by increasing recognition of childhood trauma, rising healthcare expenditure, and growing demand for evidence-based therapeutic interventions. Within this market, TYCDD represents a specialized niche with substantial potential due to its ability to address root causes of various mental health issues.
Cost-Effectiveness: Research suggests that early intervention through TYCDD can lead to long-term cost savings by reducing the need for more intensive, costly treatments in adulthood.
Healthcare System Benefits: Integrating TYCDD into healthcare systems can improve patient outcomes, reduce hospital admissions, and lower overall healthcare costs.
Family Impact: Effective TYCDD treatment can alleviate parental stress, enhance family functioning, and improve the overall quality of life for affected families.
The economic implications of TYCDD extend beyond individual cases:
Productivity Gains: By helping children overcome dissociation and trauma, TYCDD contributes to improved academic performance, higher employment rates, and increased productivity as they grow into adulthood.
Reduced Social Welfare Dependency: Effective treatment can lead to decreased reliance on social welfare programs, freeing up resources for other community needs.
Community Resilience: Strengthening the mental health of young individuals through TYCDD contributes to more resilient communities better equipped to face challenges.
Technological advancements have revolutionized TYCDD in several ways:
Online Therapy Platforms: Digital platforms enable access to therapy sessions, psychoeducation, and support groups from the comfort of home, reaching underserved populations.
Virtual Reality (VR) Therapy: VR offers immersive exposure therapy experiences, helping children confront traumatic memories in a safe, controlled environment.
Mobile Apps: Customized apps provide tools for self-monitoring, cognitive reprocessing, and psychoeducation, empowering children and their families between sessions.
Personalized Therapy: Artificial Intelligence (AI) holds promise in tailoring therapeutic interventions based on individual needs, enhancing treatment efficacy.
Remote Access: Teletherapy offers a sustainable model for delivering TYCDD to rural or underserved communities with limited access to mental health services.
Data Analysis: Wearable devices and mobile apps can gather valuable data on child behavior and progress, aiding therapists in making informed decisions.
Cybersecurity Concerns: As digital therapy tools become more prevalent, ensuring the privacy and security of sensitive patient data becomes a critical challenge.
The development and delivery of TYCDD are shaped by various policies and regulations that vary across jurisdictions:
Mental Health Legislation: Laws governing mental health services provide the legal framework for offering TYCDD, outlining professional responsibilities, patient rights, and funding mechanisms.
Data Privacy Laws: Regulations like GDPR (General Data Protection Regulation) in Europe or HIPAA (Health Insurance Portability and Accountability Act) in the USA ensure the confidentiality of patient data during digital therapy delivery.
Insurance Coverage: Policies determining insurance coverage for mental health services influence accessibility, with some plans explicitly including TYCDD as a covered benefit.
Standardization: Regulatory bodies often provide guidelines for evidence-based practices in child mental health, ensuring consistent quality and safety standards in TYCDD delivery.
Funding and Resource Allocation: Policies related to healthcare funding can impact the availability of specialized TYCDD programs, influencing accessibility for affected children and families.
Research and Training: Government initiatives supporting research and training in dissociation and TYCDD foster professional development and knowledge advancement.
Despite its effectiveness, TYCDD encounters several challenges:
Stigma and Misunderstanding: Lack of awareness about dissociation and TYCDD can lead to stigma, hindering parents from seeking help and therapists from offering specialized services.
Limited Access to Specialized Therapists: The scarcity of trained professionals in this field limits availability, especially in rural or underserved regions, creating a gap in access to quality care.
Cultural Barriers: Cultural beliefs and practices can impede the delivery of TYCDD, requiring therapists to adapt their approaches while maintaining cultural sensitivity.
Criticisms of TYCDD include:
Lack of Longitudinal Studies: Critics argue for more extensive research on the long-term outcomes of TYCDD to solidify its efficacy.
Cost Concerns: While cost-effective in the long term, the initial investment in training therapists and establishing specialized programs can be a barrier.
Addressing these challenges requires collaborative efforts:
Awareness Campaigns: Educating the public about dissociation, TYCDD, and childhood trauma reduces stigma and encourages help-seeking behaviors.
Training Programs: Expanding access to training for mental health professionals can increase the number of specialists offering TYCDD.
Cultural Competency Training: Equipping therapists with cultural sensitivity skills ensures culturally responsive practice and overcomes barriers in diverse communities.
Public-Private Partnerships: Collaborating with healthcare systems, non-profit organizations, and government bodies can help overcome funding and resource constraints.
Background: Emily, aged 8, presented with severe anxiety, flashbacks, and disassociation following a traumatic car accident. She struggled in school and had limited social interactions.
Treatment Approach: TYCDD was implemented using a multi-modal approach including play therapy, EMDR, and family counseling. Therapists used creative art to help Emily express her emotions and memories while involving her parents in sessions to enhance their understanding and support.
Outcomes: After 6 months of treatment, Emily showed significant improvements. She regained her ability to concentrate in school, started playing with peers, and reported feeling “more like myself.” Her parents noted improved family dynamics and better management of Emily’s anxiety at home.
Scenario: Michael, a 10-year-old refugee from a war-torn country, exhibited signs of dissociation and post-traumatic stress disorder (PTSD). He had difficulty sleeping, experienced flashbacks, and displayed emotional detachment.
Therapeutic Intervention: A team of psychologists and social workers employed TYCDD, incorporating elements of play therapy and cultural sensitivity. They created a safe space for Michael to express his experiences through art, helping him process trauma and reconnect with his emotions.
Results: Over several months, Michael’s symptoms gradually decreased. He became more engaged in school activities, improved his communication with peers, and regained a sense of hope for the future. His family reported feeling closer as they navigated their new life together.
Setting: A rural community in Africa faced challenges addressing dissociation in children due to limited resources and cultural barriers.
Initiative: Local non-profit organizations, in collaboration with mental health professionals, developed a community-based TYCDD program. This approach involved training local leaders and caregivers on recognizing dissociation and providing basic interventions.
Impact: The program empowered communities to support vulnerable children, reducing the burden on formal healthcare systems. It fostered cultural sensitivity, ensuring that therapeutic practices aligned with traditional beliefs while addressing dissociation effectively.
The field of TYCDD continues to evolve, shaped by emerging trends:
Integrative Approaches: Combining TYCDD with other therapeutic modalities, such as mindfulness or neurofeedback, offers comprehensive treatment options for complex cases.
Digital Transformation: The integration of AI, VR, and mobile technology will likely drive further innovation in therapy delivery, personalization, and accessibility.
Cultural Fusion: Therapists are increasingly blending traditional cultural practices with evidence-based TYCDD techniques to create culturally responsive interventions.
To capitalize on these trends and ensure the continued growth and effectiveness of TYCDD:
Research Collaboration: Encouraging interdisciplinary research collaborations fosters innovation, improves treatment protocols, and addresses knowledge gaps.
Global Knowledge Sharing: Establishing platforms for sharing best practices and success stories across cultures can enhance global understanding and implementation of TYCDD.
Policy Advocacy: Advocating for supportive policies and funding mechanisms ensures the sustainability and accessibility of TYCDD services worldwide.
Therapy for Young Children Dissociative Disorder represents a powerful tool in the arsenal of child mental health professionals, offering hope and healing to countless young lives. By understanding its core components, global impact, economic considerations, technological advancements, policy frameworks, and challenges, we can appreciate the intricate web of support it provides. The case studies presented illustrate the transformative potential of TYCDD, emphasizing its role in fostering resilience and restoring function in affected individuals.
Looking ahead, the future of TYCDD appears promising, with emerging trends pointing towards even more effective and accessible interventions. As technological innovations mature, collaborative efforts across cultures and jurisdictions will be crucial to ensure that these advancements reach those who need them most. By investing in research, training, and supportive policies, we can continue to cultivate a global community that prioritizes the mental health and well-being of young people, ensuring they thrive into adulthood.
Q: What is dissociation?
A: Dissociation is a complex psychological mechanism where an individual feels detached from their thoughts, feelings, memories, or surroundings. It can range from mild feelings of detachment to more severe experiences of amnesia or altered identity.
Q: How do I know if my child might be experiencing dissociation?
A: Signs may include sudden changes in behavior, difficulty concentrating, flashbacks or nightmares, emotional volatility, and a sense of detachment from the self or environment. However, only a qualified mental health professional can diagnose dissociation or dissociative disorders.
Q: Is TYCDD suitable for all children with dissociative symptoms?
A: While TYCDD is a promising approach for many, its effectiveness depends on various factors, including the child’s age, severity of symptoms, cultural background, and access to specialized therapists. Individualized assessment and treatment planning are crucial.
Q: Can TYCDD help adults who have experienced trauma?
A: Yes, TYCDD can be adapted for adults and is often used in conjunction with other therapies for complex PTSD or traumatic memory disorders. However, the specific approach may vary depending on age and individual needs.
Q: Are there any risks associated with TYCDD?
A: As with any therapy, there are no guarantees of immediate improvement. TYCDD involves a collaborative process where therapists work closely with children and families to ensure safety and well-being throughout treatment. Potential risks are minimal compared to the benefits achieved for many individuals.

Dissociative disorder in young children, often stemming from trauma, causes them to detach from real…….
Dissociative disorder in young children, arising from trauma, causes emotional disconnection and fra…….